RESULTS
Give your feedback!
What is QT interval?
The QT interval is an electrocardiogram measurement to assess some of the characteristics of the electricity of the heart. It is measured as the time from the beginning of the Q wave to the end of the T-wave and close to the time from when the chamber of the heart begins to contract after completing relaxation. An unusually short or long interval is correlated with the chance of creating abnormal heart rhythms and immediate death of the heart. QT interval abnormalities can be caused by genetic disorders such as long QT syndrome, certain drugs, and blood salt disorders such as hypokalaemia or hypothyroidism due to hormonal disorders.
How QT interval is measured?
The QT interval for serial ECG evaluation is most often measured in lead II, while leads I and V5 are comparable to lead II. In order to measure the QT interval, leads III, V1 and aVL are usually avoided. Precise QT interval calculations are subjective because the end of the T wave is not always well defined and gradually joins the baseline. The QT interval in an ECG complex can be manually measured using various methods, such as the threshold method, where the end of the T wave is defined by the point at which the T wave component merges with the baseline isoelectric. Or the tangent method in which the T- wave end is defined by the tangent line intersection coming to the isoelectric baseline from the T wave at the maximum drop point.
Why Bazett's formula?
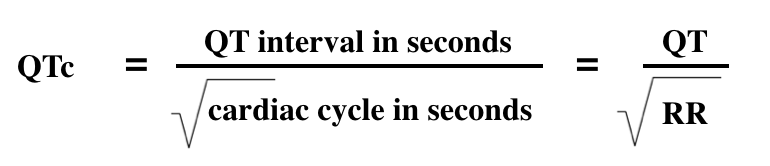
The most commonly used formula for QT correction is the Bazett formula, named after Henry Cuthbert Bazett( 1885- 1950), a physiologist who invented it to calculate the heart rate-corrected interval (QTcB) of QT. The formula of Bazett was based on the observations of a 1920 study. The correct mathematical form of Bazett's formula is:
Where QTcB is the heart rate QT interval, and RR is the interval between the onset of one QRS complex and the onset of the next QRS. This mathematically correct formulation returns QTc generally in milliseconds in the same units as QT. This formula, in some popular forms, measures QT in milliseconds and RR is measured in seconds, often derived from the cardiac frequency (HR) as 60/HR.
Causes for Abnormal QT intervals
Prolonged QTc causes the potential for premature action during the late depolarization phase. This increases the risk of developing fatal ventricular fibrillation, including ventricular arrhythmia. In women and older patients, high systemic blood pressure or heart rate and short stature and higher rates of prolonged QTc are seen.
Prolonged QTc values are also associated with ECG findings are known to degenerate into ventricular fibrillation associated with higher mortality rates called Torsades de Pointes. Many other causes for prolonged QT intervals are more common than genetic causes.
Genetic Reasons:
Prolonged or abnormal QT interval may be caused by a long QT syndrome, while a short QT interval may be caused by a short QT syndrome. The length of QTc is associated with variations in the NOS1AP gene. Jervell and Lange-Nielsen autosomal recessive syndrome is characterized by a prolonged QTc interval in combination with sensory hearing loss.
Mortality Predictor:
Electrocardiography is a noninvasive and safe tool for identifying people with higher death risk. There was no consistent evidence in the general population that the prolonged QTc interval in isolation is associated with an increase in death due to cardiovascular disorder. However, multiple studies found the abnormal QT interval as a demise predictor for diseased population subsets.
Adverse reactions of Drugs:
The QT interval can be prolonged due to adverse drug reactions. Many medications, such as ziprasidone, haloperidol, methadone, sertindole, and vemurafenib may prolong the QT interval. Some drugs, such as sotalol or amiodarone (use for antiarrhythmic), work by obtaining pharmacological QT prolongation. Some antihistamines of the second generation like astemizole also have this effect. Moreover, high concentrations of blood alcohol extend the QT interval. A possible interaction with QT prolongation is associated with selective serotonin reuptake inhibitors and thiazide drugs. There is no doubt that macrolide antibiotics extend the QT interval after it was recently discovered that azithromycin is linked with the increase in cardiovascular death.
Pathological Conditions:
Hypothyroidism, a condition of the thyroid gland 's low function, can cause to prolong QT. Acute hypocalcemia causes the QT interval to prolong and can lead to ventricular dysrhythmia. A reduced QT can be associated with hypercalcemia.
Rheumatoid arthritis:
The most common inflammatory arthritis is rheumatoid arthritis. Studies have associated rheumatoid arthritis to more cardiovascular disease deaths. In a study in 2014, Panoulas et al. found that the death ratio in patients with a lower QTc interval had lowest mortality rates while the QTc interval (> 424 ms) had higher mortality rates. The association lost when the calculation for the level of C-reactive protein was corrected. The analysts recommended that inflammation increased the QTc period and produced arrhythmias that were related to higher death rates. The mechanism by which the C- reactive protein is linked to the QTc interval is not yet understood.
Diabetes Type 1:
Type 1 diabetes can increase the risk of mortality compared to the general population. Nearly half of patients with type 1 diabetes have an abnormal QTc (> 440 ms) interval. 29% mortality has been related with diabetes with prolonged QTc interval. In contrast with 19% mortality with common QTc interval. Antihypertensive drugs have increased the QTc interval but have not been an independent mortality predictor.
-
Total Reviews 0
-
Overall Rating
0/5
- Stars
Thank You! For Your Review
Your Review Will Appear Soon.